An important part of the gender transition journey is gathering information to help you to make the choices that are right for you. The journey may also include counselling for clarity, lifestyle changes, hormone treatment, and even surgery.

Who may benefit from Gender Affirming Hormone Therapy?
Gender affirming hormone therapy (GAHT) is a very personal decision. There is a lot to think about, and whilst it is great that there is growing information available, this can also make it confusing to know where to start! So here’s a quick summary of what gender-affirming hormone treatment (GAHT) is, what to think about, and what to expect – written by your friendly ERH endocrinologists.
Every persons experiences and preferences when it comes to gender identity are valid, and we are becoming more and more aware of the different ways people can experience gender identity. We no longer have to fit into a binary category of male or female if that doesn’t feel right. We won’t discuss all the different gender identities here, but what we want to do is give you an idea of what GAHT is, what it can do, how it is used, and what to do next if you are interested in finding out more about whether GAHT is right for you.
First up, we’d like to say, there’s no right or wrong way to do this! Some trans people choose not to use hormone therapy, whilst some non-binary people use some hormone therapy. There are no absolutes around GAHT timing; there isn’t an upper age limit, and there are no absolute rules in terms of when to move through to the next step in your gender affirmation journey. For some people, GAHT can be a very useful tool to relieve the distress that can come with a discrepancy between gender identity and the gender assigned at birth.
When can Gender Affirming Hormone Therapy be started?
Those of us that are working in the area of GAHT consider two broad aspects of care prior to hormone commencement as part of a holistic overall approach:
- The first is readiness to use hormone therapy – both psychological and physical readiness
- The second is the safety of hormone therapy and how to provide the safest regimen possible.
GAHT is a big step, and the journey can be challenging. Whichever route you take to accessing GAHT, collaboration and informed decision making are important. Before starting GAHT, it is important to have a discussion about the types of treatment options and the expected effects of those treatments. This discussion will help you to clarify your goals of treatment and decide if GAHT is right for you. It may involve seeing a psychologist or counsellor skilled in this area. In addition, the psychologist/counsellor may provide you with support over the transition time. Even the most successful transition has “bumps in the road” and support from health professionals as well as whanau or family and friends is important.
Before prescribing GAHT, doctors consider a variety of general health information such as other medical problems, medication and any family history of medical problems. Just like any other medications, GAHT has the potential for some risks and side effects, and the risks can be higher in certain contexts. For example, do you smoke or vape? GAHT can increase the risk of blood clots, as can smoking. How much alcohol do you drink? Any other drug use? Exercise? Then doctors consider your blood pressure and weight. You may be asked to have a blood test. This information helps us make decisions about the safest hormone therapy regimen. Medical issues such as a previous blood clot and heart issues are also important for your doctor to consider and discuss carefully with you prior to starting treatment.
What about fertility?
Fertility can be affected by GAHT, so prior to starting your doctor will discuss whether you wish to have fertility preservation. Again, it’s important to discuss this with medical professionals who work in this area all the time, as they understand that sometimes fertility may not be something that you want or have thought about at the time of coming forward for GAHT, but can talk you through the options for preserving the option for fertility in the future.
Receiving feminising treatment
If you are assigned-at-birth-male and planning feminising treatment, there is the option to preserve sperm prior to feminising treatment. This is a reasonably simple procedure and involves producing sperm into a cup. The lab will freeze the sperm for you and save this. In New Zealand semen can be frozen for 10 years and then after this permission needs to be obtained from the fertility ethics committee (ECART) for longer preservation. This procedure has public funding in New Zealand if certain criteria are met; the criteria are that you are a New Zealand resident and don’t already have any of your own children, you are younger than 40 years and are undergoing treatment that permanently impairs fertility in the public system.
Receiving masculinising treatment
If you are assigned-at-birth female and starting masculinising treatment, prior fertility preservation involves freezing oocytes (eggs). This is a more complicated procedure that involves undergoing the first part of an in-vitro fertilisation (IVF) cycle;. This means that your ovaries are stimulated with hormones and with the aim to maturing group of eggs. These eggs are then removed through the top of the vagina and put in the freezer. These eggs can be frozen for 10 years in New Zealand but further permission can be obtained from the fertility ethics committee (ECART).
Hormone therapy commencement:
There are different ways to start hormone therapy and different ways of administering hormones, we don’t yet have medical studies comparing these different regimens to know which is the best one. A good way to think about this process is that it is like a second puberty. There are good reasons not to rush this process, and usually doses start low and then slowly increase. There can be side effects to hormones that are better tolerated if doses are slowly increased. This process of slower dose increases also allows time to adjust to these changes in your life.
Feminising GAHT
Funded Estrogen in New Zealand involves either an oral tablet (progynova) or a patch (estradot). Other products available overseas (with no funding in New Zealand) include estrogen gels, spray, injectable estrogen or estrogen pellets that typically are placed every 6 months. Doses are typically increased every 6 months and hormone levels are monitored with a blood test initially 3 monthly. The tablet form of estrogen is associated with a small increased risk of clot in the legs and the lungs.
Masculinising GAHT
When starting masculinising treatment often the first step is to start testosterone tablets or very low dose injections. In New Zealand funded options include oral tablets (andriol), 3 weekly injections (sustenon), 3 monthly injections (reandron) or a testosterone patch (androderm). Doses are adjusted every 3 -6 months depending upon masculinising effects and hormone levels (monitored by a blood test). Frequency of blood testing depends on which product you are using and how fast doses are being adjusted. Side effects can include acne, aggression and a increase in libido.
Further information will be provided by your doctor in your appointments and they will also provide information about the long term risks and monitoring of therapies.
Finding out more
Talk to as many supportive people as you can and read relevant resources. But remember, your gender-affirmation journey might look different to anyone else’s, and that is ok. Different medical providers can help with hormone transition. Some people get support from their general practitioner for hormone therapy. Others access the public trans gender care clinic for hormone therapy commencement. There are sexual health physicians and endocrinologists (hormone specialists) working in this area. Collaboration and shared decision-making are important.
If you are interested in taking the next step, see your doctor for further information and a discussion to consider long term benefits and risks.
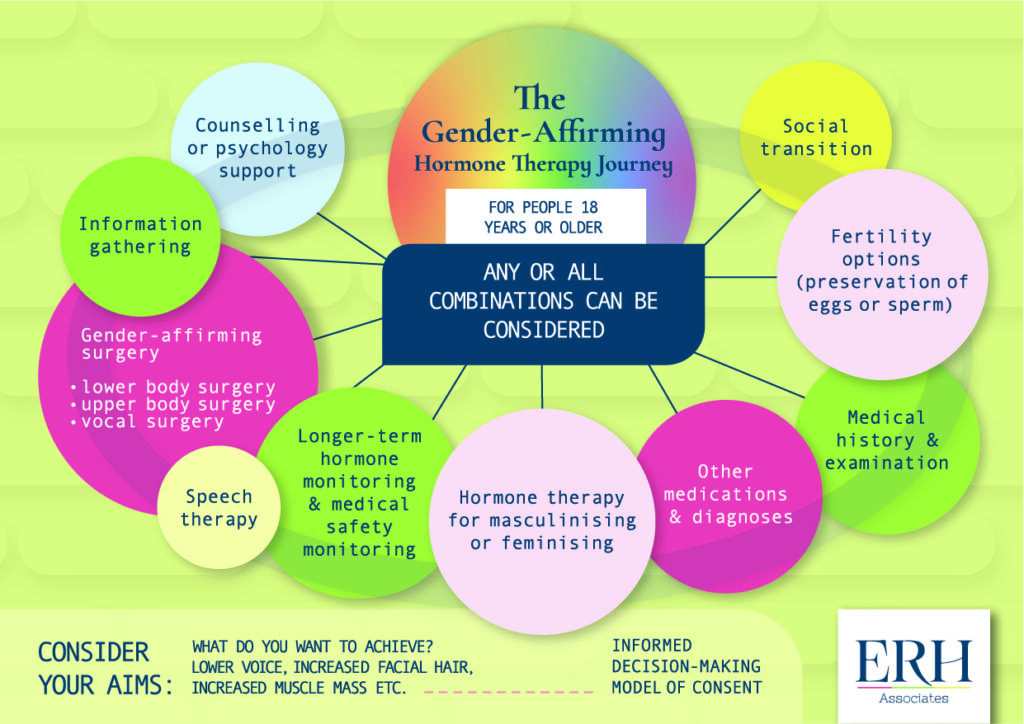
You can also download a free copy of the below infographic from the erhassociates.co.nz home page
Comments +