What happens during biological sexual development?
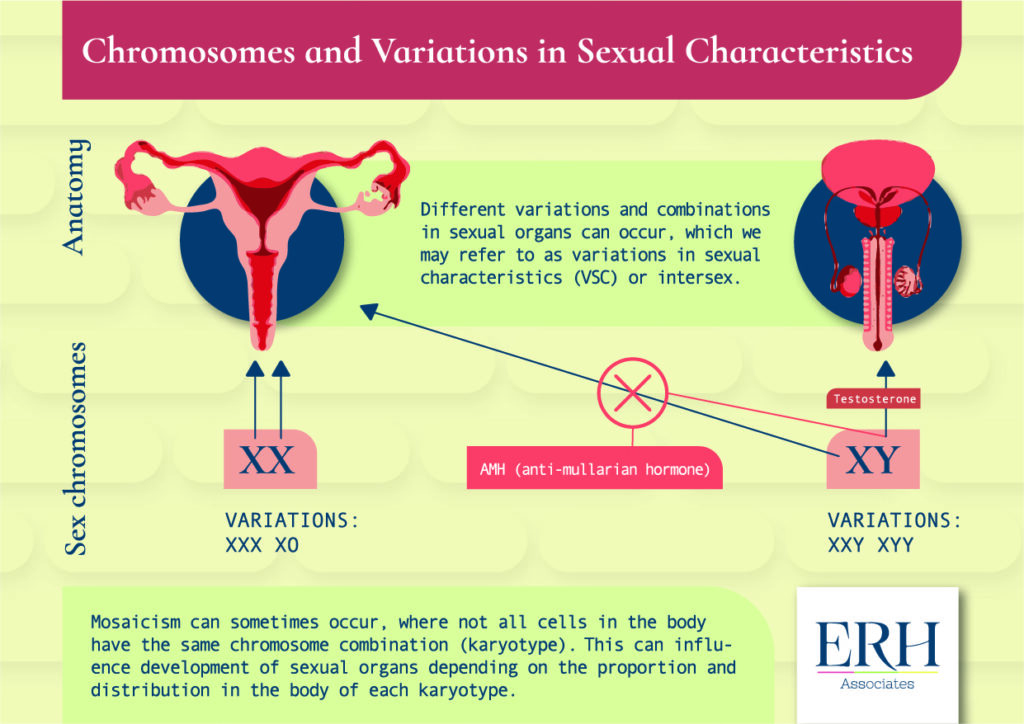
In assigned-at-birth women/girls the sex chromosomes present are usually two X chromosomes (XX) and these chromosomes are involved in the development of the vulva, vagina, uterus, ovaries, fallopian tubes, and associated structures. In assigned-at-birth men/boys, the usual sex chromosome pattern is to have one X and one Y chromosome (XY).
The “default” biological development process in humans is for the X-chromosome to allow vulva, vagina, uterus, ovaries, fallopian tubes, and associated structures to develop. However in assigned-at-birth-men/boys, the Y chromosome usually leads to the secretion of high levels of testosterone which allow the development of penis, testes, scrotum and associated structures, and the secretion of Anti-mullerian Hormone (AMH) which suppresses the development of ovaries, uterus and other associated structures in assigned-at-birth men/boys.
What is VSC (Variation of Sexual Characteristics) or Intersex
Different variations or combinations in genitals and internal sexual organs can sometimes occur, which we may refer to as Variations in Sexual Characteristics (VSCs) or Intersex. These variations can be related to differences to the usual combination of sex chromosomes, changes to how enzymes in the body usually work to produce sex hormones or changes to the biochemical receptors to sex hormones in the body.
VSCs are usually noted at birth but for some people only become apparent at puberty when sex hormone levels increase. VSC probably occur in up to 2% of the population.
What other terms might you hear that are used for VSC or Intersex?
Different terminology have been used. An older term is “DSD” -this is no longer used to stand for Disorders of Sexual Development and now stands for Differences in Sexual Development when it is used, in recognition that these variations are normal for the people who have them.
What types of VSC are there?
Biologically, VSC can be divided into categories depending on how they occur. These include
-Congenital adrenal hyperplasia (CAH) where reduced activity in an enzyme involved in hormone formation leads to reduction in some adrenal hormones but higher testosterone levels. This can lead to an assigned-at-birth woman/girl being virialized (developing some features which may usually be associated with assigned-at-birth men/boys).
-Another example of VSC in a person who may have been initially been assigned-at-birth as female, is “androgen insensitivity”. Here a person with XY sex chromosomes (which usually leads to the development of the penis and associated structures) has sexual characteristics that would usually be seen externally in assigned-at-birth women/girls, because although testosterone is produced, the usual effects on the body don’t occur, because the testosterone receptors aren’t working in the usual way. Internally, the uterus and may be absent because AMH is still produced which suppresses the development of these structures. The testis may be inside the abdomen rather than outside the body, in which case surgery will usually be recommended, because testes that are situated inside the pelvis/abdomen have a small chance of developing cancer cells. The prospect of surgery can often come as a shock, and discussion with your medical team which may include an expert counsellor can be very helpful.
-There are also sex chromosomes combinations where the external genitalia can appear typical for an assigned-at birth female, for example Turner syndrome where there is only one X chromosome (XO). In the case of Klinefelter syndrome (XXY) penis and external testes usually develop. These chromosome variations have certain biological effects.
You can read more about different types of VSC on the Intesex Aotearoa website here.
How is VSC identified?
When the possibility of VSC has been raised, the health team will usually undertake some blood tests, checking hormone levels and then sex chromosomes. Sometimes, when the chromosome combination does not match the physical appearance, this can be a surprise to the person with the VSC and/or their parents. Counsellors expert in this area can be helpful in guiding you in processing this information and make decisions in your care. There may be some more genetic testing needed for clarification, and imaging (such as ultrasound and/or MRI) may be undertaken to look at the internal sex organs.
All of these assessments can take time and specialist input is usually recommended, required, either a paediatric or adolescent endocrinologist and a gynaecologist or urologist. If you live rurally, it may be necessary to travel to a specialist unit or receive care remotely via telehealth.
The diagnosis of VSC doesn’t necessarily mean that any particular course of action is required. It is a finding, not a treatment plan, however, for some VSC, particular treatments may be recommended for your health. For example testes that are situated inside the pelvis can be prone to developing cancer cells (as opposed to outside in the body in a scrotal sac ), so surgery is usually discussed in this situation. Another example when medical treatment might be required is if ovaries are only partially formed and therefore don’t produce enough oestrogen to provide the usual health benefits such as supporting normal bone density. In this situation, oestrogen-containing hormone treatment is usually recommended.
Once the health team are confident of the type and features of the VSC, then treatment options can be considered. In addition to considerations to health such as those discussed above, healthcare for people with VSC may including gender-affirming treatment. Where possible, gender-affirming treatment is often deferred until a child is old enough to make decisions for themselves.
Navigating the diagnosis and living with a VSC can be complicated. In addition to health considerations, access to good resources is important for optimal care and support from a sociocultural and psychological perspective. The Intersex Aotearoa, website is a helpful resource run by a non-profit organisation that provides resources and advocacy for individuals, parents and whanau.
Resources and links for further information
https://www.intersexaotearoa.org
You can also download a free copy of our infographic below from the erhassociates.co.nz homepage.
Comments +